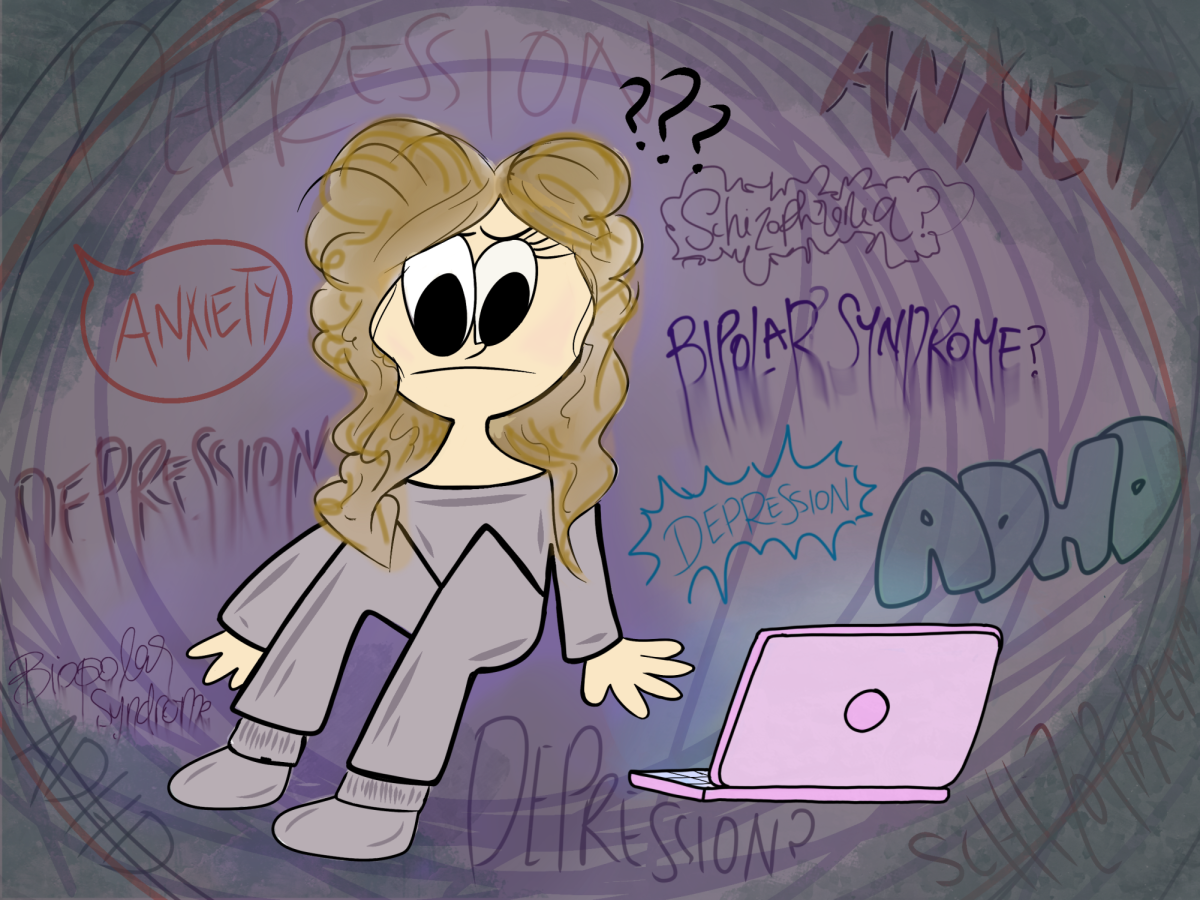
Though a stigma still exists, awareness around mental health has been raised, especially with younger generations getting vocal about such topics on social media to rid the pre-existing view of its “taboo.” This has also opened the door to conversations concerning mental health disorders such as Attention Deficit/Hyperactivity Disorder (ADHD), anxiety, depression, Obsessive Compulsive Disorder (OCD), bipolar syndrome, and schizophrenia.
While this development has led to positive changes with more resources and tools being available to people struggling with these disorders, it seems like the overflow of information about mental health online has led us to become hyper-aware of these illnesses. Sometimes, this leads to self-diagnosing a disorder by miscategorizing symptoms when they could be the effects of other issues a person is struggling with. While these labels may provide comfort or a deeper understanding of oneself, being overdiagnosed with a mental health disorder that is nonexistent is dangerous.
According to the Centers for Disease Control and Prevention (CDC), over one in five 13 to 18-year-olds are currently experiencing a mental health illness or have struggled through a mental health problem/crisis, and one in five U.S. adults are currently living with one, as of 2023. This surge in mental health disorder diagnosis seems to correlate with a surge in misdiagnosis by doctors who assign a patient’s symptoms to the wrong disorder, or patients themselves who self-diagnose their conditions based on boxes they think they fit in.
Both can lead to a worsening in condition by taking the wrong medication and creating a limited mindset, which is essentially when patients tell themselves they feel/should act a certain way or are unable to perform a task because they have been diagnosed with a disorder, limiting their abilities.
Creeping into Medical Reports: Over-diagnosis
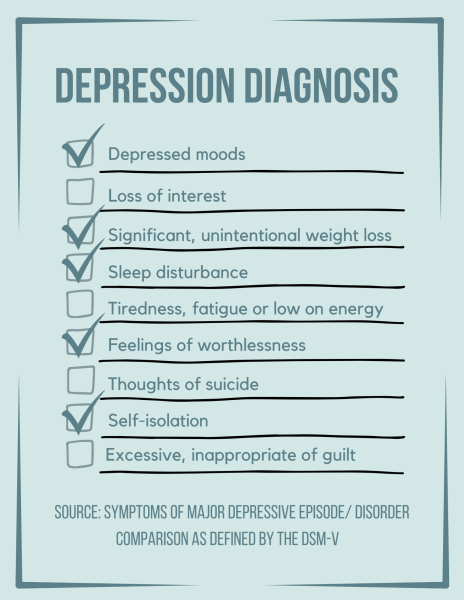
When diagnosing mental disorders, doctors follow the Diagnostic and Statistical Manual for Mental Disorders (DSM-V), a classification system with criteria to describe such disorders. According to the DSM-V, a patient must check at least five symptom boxes to be diagnosed with depression. Among them are symptoms like being in a depressed mood, significant weight loss or gain in short periods, sleep disturbance, loss of interest, and self-isolation. Many of these symptoms can also be used to describe a variety of other mental health disorders, such as bipolar syndrome, which entails characteristic depressive episodes.
Misdiagnosis leads to the prescribing of the wrong medication and treatment plans that won’t work. With disorders like Bipolar syndrome, a misdiagnosis of depression can cause physical and mental damage, while also being dangerous.
Dealing with life’s challenges and traumatic experiences can be especially daunting for teenagers, and analyzing symptoms of stress or natural reactions to difficult circumstances may also lead to one’s misinterpretation of symptoms, and eventually over-diagnosis. When patients self-assess whether they have symptoms, assessments can be skewed depending on how they view themselves and what they think they are experiencing.
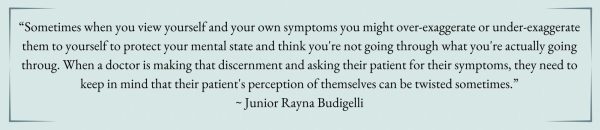
Junior Rayna Budigelli thinks it is important to consider that a patient’s perception of themselves may lead to over-diagnosis. “Sometimes when you view yourself and your own symptoms you might over-exaggerate or under-exaggerate them to yourself to protect your mental state and think you’re not going through what you’re actually going through,” Budigelli said. “When a doctor is making that discernment and asking their patient for their symptoms, they need to keep in mind that their patient’s perception of themselves can be twisted sometimes.”
Misclassification of symptoms, assigning them to the wrong disorder, and wrong interpretations of a patient’s symptoms, prove that it is hard to identify a patient’s mental health disorder.
Even if it’s the wrong disorder and the medication only makes the condition worse, we start to identify with, or “become one with” the disorder, and set personal limits for ourselves when thinking that we are incapable of achieving our full potential because of the disorder.
Checking All the Boxes: Self-Diagnosis
As an alternative way to dealing with mental health struggles, some teens turn to the online world of information and social media in search of a better understanding of themselves and their condition, or for simply finding safety in a group of peers struggling with the same problem. However, the overflow of unreliable, often incorrect, and misleading information found on vlogs and health sites may lead someone trying to look for an answer for why they feel out-of-place or unhappy to identify with a disorder that they don’t have. This can happen when they read about symptoms that they believe apply to them and then self-diagnose themselves.
Junior Michelle Rowberry did some research looking into the signs of anxiety, after she experienced a panic attack, to find answers. “[Researching anxiety’s symptoms] definitely affirmed ‘I think I have anxiety’, and then it was like ‘oh no I have anxiety, I have to panic about that’, and that’s gonna make you feel more anxious, and it’s not gonna help, it’s just gonna confuse the whole thing,” Rowberry said. “[With depression], you’ll assign yourself to sadness and be like ‘that’s just what I do now’, that’s going to be really bad for your mental health.”
Budigelli agrees with Rowberry; for her, identifying with a self-given label of having a mental health disorder is like setting fire to the flame. “You just start fueling yourself since you take on that role of ‘Oh I have this thing’,” Budigelli said. “You start exhibiting those symptoms more because you think you should, but since you are exhibiting those symptoms more, you realize ‘Oh, I actually do have this.’ It’s a never-ending cycle.”
What Should We Do About it?
While over-diagnosis is one part of the problem, sometimes, being incapable and afraid to face the situation is a more dangerous problem, leading to suicide or substance abuse to relieve from a seemingly never-ending mental battle one can’t combat on one’s own. According to the findings of a longitudinal study (1999-2016) published by the CDC, 46% of people who died by suicide also struggled with a mental health condition. Overdiagnosis where there is no mental health disorder, can limit one’s mindset and abilities, or worsen conditions, but hesitating to reach out for help or verification of an assumed disorder is dangerous.
Rock Ridge provides students with a great amount of resources to help them cope with mental health struggles. A student can make an appointment with their guidance counselor, school psychologist, or social worker, or reach out to programs like PEER and Sources of Strength to seek help.
It is equally as important to trace more defined lines between feeling down because of everyday stresses and having a mental health condition. We can change how we view our mental health and everyday struggles by looking for more opportunities for improvement and growth, rather than pushing responsibility away because of the boundaries mental health disorders set lacklusterly.









![Held up by a group of cheerleaders, flyer sophomore Leyu Yonas poses as part of a stunt, also supported by flyer junior Shayne Mitchell behind her. (Left) Prior to the pink out football game on Oct. 13, the athletes practiced in the aux gym from 5 p.m. to 6:30 p.m. (Right) On Oct. 19, the cheerleaders competed in their District Championships at Woodgrove High School. “We definitely put all our effort on the mat [at Districts], and it showed,” Mitchell said. Left: Photo by Nadia Shirr. Right: Photo by Steve Prakope via Victor O’Neill Studios.](https://theblazerrhs.com/wp-content/uploads/2023/11/feature-image-1200x823.png)
![Sophomore Xavier Smith (6), the Phoenix quarterback, runs the ball as his teammates help hold up the defense. “My [offensive] line collapses, so I just [have to run], and its a good way to get first downs because [Tuscarora’s] defense was really good,” Smith said.](https://theblazerrhs.com/wp-content/uploads/2023/11/IMG_5383-1200x897.jpg)



![As the referee throws the ball up for the tip-off, freshman Simone Diby leaps towards the ball to get it in Phoenix possession. Diby is a new member of the Phoenix girls basketball team, and despite it being a change, she finds it enjoyable. “It’s definitely a different experience if you’ve never played on a team, [but] I think it’s still fun.”](https://theblazerrhs.com/wp-content/uploads/2024/03/DSC_0057-1200x662.jpg)




















Jim Vincent • Feb 18, 2024 at 1:03 pm
I think that the onus is on the psychiatrist to correctly diagnose mental illness, and primary care doctors need to responsibly make sure the patient gets to one.
Too many times primary care doctors are too quick to diagnose and treat mental illness that they don’t have the proper training to diagnose.
The influx of internet misinformation is of coarse also a major factor.
Vearry Hale • Feb 18, 2024 at 11:29 am
Many people have been violated of the constitution of rights that are black and brown, who requested services waiting for 50 minutes EMS don’t show up the police show first they find out you are a person of color and violating your constitutional rights cause you asked for services and police officers are able to use access to force violating the persons constitution of rights, denying you depriving you from getting services which is unconstitutional when it comes to rules regulations, protocols and policies, they must examine the police officers who can make pranks and hold them accountable, and make sure transparency because people don’t deserve to go to jail of prison when they followed the law and our police officers are racist and discrimination It black and brown people can’t get services like others. I’m tired of them making example out of black and brown people who follow the law please officers should never get away with committing crimes like this and the only hurts the victim. Who is suffering and it is appalling when a parent has to see all of this happen, and notice the system has failed. You could never get your freedom back the way you had it your livelihood the way you supposed to win the system has failed you we living in a society with many people have to even be careful, when they need help, no one should have to go to jail or prison, and have not committed to crime but suffering from illness we know the system is broken, but we will continue to fight and make sure people get services and our community because every life matters, and it must be transparency